Low Back Pain and Degenerative Disc Disease
Low Back Pain
Low Back Pain and Degenerative Disc Disease , Low Back Pain son derece yaygındır ve insanları hekime götüren en önemli hastalıkların ikincisidir. İş gücü kayıplarının en sık rastlanan sebeplerinden biridir. Ömür boyu görülme sıklığı %60-80 arasında değişir. %1-3’ü cerrahi girişim gerektirir. Büyük çoğunluğu 2-3 hafta içinde iyileşir. Nasıl tedavi edilirse edilsin hastaların %70 inde tekrarlar. Low back pain The prognosis is good in most cases and recovery usually occurs with little or no medical intervention. It occurs in all ages and genders.
Definitions
Radiculopathy
Any pressure or damage to the nerve roots coming out of the spinal cord nerve root It is the presence of symptoms such as pain, tingling, numbness, loss of sensation and strength in the distribution area of the nerve as a result of damage for any reason.
Sciatica
It is a lesion of the thickest and longest nerve in the body, resulting from radiculopathy of a nerve root (L4, L5 or S1) that joins the sciatic nerve. Radiculopathy symptoms extending along the back and side of the lower extremity to the foot and ankle.
Mechanical low back pain
Spinal circumference your muscles and/or strain on ligaments, irritation of facet joints low back painIt is the most common form of low back pain, excluding anatomically determinable causes (e.g. tumor, disc herniation).
Radiological evaluation
Direct graphs
A variety of clinically significant congenital anomalies may be detected (e.g. spina bifida occulta). Spinal malignancy, infection, inflammatory spondylitis, or clinical It is useful for patients who are likely to have significant fractures. Surgical indications for disc herniation and spinal stenosis cannot be made from plain radiographs.
Findings supporting disc disease (flattening of lordosis, scoliosis, decrease in intervertebral disc height) may be seen. It is useful in showing movement instability. It may not give any findings of disc disease.
MRI : The structure of the intervertebral disc and the width of the spinal canal provide valuable information about spinal tumors. The cauda equina is evaluated in sagittal images. It provides better information than CT about tissues outside the spinal canal (e.g. extraforaminal disc herniation, tumors…).
BT : If technically sufficient images are obtained, they may be sufficient to recognize most spinal pathologies. They provide better information about the bone structure.
Lumbar Disc Herniation (Lumbar Disc Herniation)
Anatomy: The intervertebral disc is located between two vertebral bodies and acts as a shock absorber. is textureIt is bordered by the soft, gelatinous nucleus pulposus in the middle, the hard annulus fibrosus around it, and the cartilaginous end plate on the surface facing the vertebral body.
Anulus fibrosusun dış yaprakçıklarındaki lifler omur cisminin epifizine direkt olarak yapışır. Bunlar Sharpey lifleri olarak bilinir. İç lamellerdeki fibriller direkt olarak kartilaginoz end platelere yapışır. Nükleus pulposus intervertebral diskin hacminin %40’ını oluşturur. Erişkin diski damarsızdır. End plate ler ve anulus etrafındaki kapillerlerden diffüzyonla beslenir.
Nucleus pulposus; kollajen lifler, proteoglycan ve su (çocukluk çağında %80) içerir. Diskin normal hidrasyonu; proteoglycan matriks tarafından osmotik olarak sağlanır (chondroitin sulfat ve daha az oranda keratin sulfatın hydrophilic zincirleriyle). Yaşın artmasıyla; chondroitin sulfatın keratin sulfata oranı azalır. Bu da diskin sıvı içeriğinin azalmasına neden olur.
Annulus fibrosus; It is composed of collagen fibers in layers.
End plate (contact surface between the disc and the vertebra); composed of hyaline cartilage.
Innervation: Sinovertebral nerves; innervate annular fibers, posterior part of disc, dura, post. long. ligament. Primary dorsal ramus; innervate facet joints, paraspinous muscle and interspinous ligament. Gray ramus; innervate anterior part of disc, ant. long. ligament.
Disc herniation (herniation) : the escape of the nucleus pulposus into or out of the tears in the annulus fibrosus. This is either a traumatic event or a structural and age-related
related degeneration. Intervertebral disc Up to 18 years old It is fed by arterial blood. At the end of the 20s and the beginning of the 30s, the entire nucleus pulposus and most of the peripheral part of the annulus fibrosus cease to receive vascular nutrition. After this age, it is fed by diffusion from the environment.
The water content of the nucleus pulposus decreases and the natural elasticity of the disc is impaired. Thus, it transmits forces in a non-linear and asymmetrical manner. The annulus becomes brittle and vulnerable over time and the nucleus loses water Fragments fragmentation facilitates herniation. For this reason, disc herniation is more common in middle ages (40-50 years old). It is rare before the age of 20.
Risk factors; obesity, smoking and poor physical conditions.
Moving and not moving The transition zone between the zones is subjected to greater pressure during movement. Thus, degenerative changes are more common in the lower cervical and lower lumbar intervertebral discs in humans.
There are 3 phases of disc degeneration
First phase : (dysfunctional phase): Various degrees of acute injury occur in the disc.
Second phase: (unstable phase): The disc space narrows and the ligaments loosen. As a result, the posterior joints of the spine (facet joints) become loosened, and the facet capsule and ligamentum flavum hypertrophy occur.
Third phase: (stabilization phase): Movement decreases.
 The nucleus pulposus can herniate in any direction out of its normal configuration. Because the nucleus pulposus is located partly posteriorly, and the annulus fibrosus has fewer lamellae posteriorly, and because the posterior longitudinal ligament strengthens the annulus fibrosus in the posterior midline, most disc herniations occur in the posterolateral direction. Central, foraminal, and, much less frequently, extraforaminal (%7-12) herniations may occur.
The nucleus pulposus can herniate in any direction out of its normal configuration. Because the nucleus pulposus is located partly posteriorly, and the annulus fibrosus has fewer lamellae posteriorly, and because the posterior longitudinal ligament strengthens the annulus fibrosus in the posterior midline, most disc herniations occur in the posterolateral direction. Central, foraminal, and, much less frequently, extraforaminal (%7-12) herniations may occur.
If it herniates from the cartilaginous plate to the adjacent vertebral body in the upper and lower directions, it is called Schmorl's nodule. It can generally be found incidentally in radiological examinations or autopsy, and has no clinical significance. Most patients with lumbar degenerative disc disease have back pain as the first symptom. This pain syndrome occurs when the annulus balloons due to the pressure of the nucleus pulposus, causing pressure on the sinovertebral sensory nerves located posteriorly. It causes radicular pain and motor and/or sensory changes by compressing the nerve root. Inflammation in the nerve root increases symptoms.
Posterolateral disc protrusion or disc extrusion often compresses the nerve root exiting the dural sac at the same distance. Left L4-5 disc herniation compresses the left L5 nerve root, and left L5-S1 disc herniation compresses the left S1 nerve root. Rarely, an upper or lower nerve root may be compressed.
Posterolateral disc protrusion or disc extrusion often compresses the nerve root exiting the dural sac at the same distance. Left L4-5 disc herniation compresses the left L5 nerve root, and left L5-S1 disc herniation compresses the left S1 nerve root. Rarely, an upper or lower nerve root may be compressed.
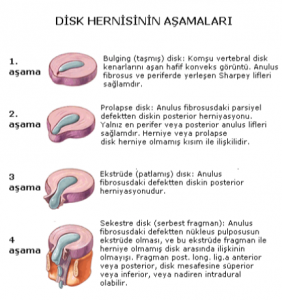
Classification of disc herniations
Bulging disk: Slightly convex image extending beyond the adjacent vertebral disc edges. Annulus fibrosus and Sharpey's fibers located in the periphery are intact.
Prolapsed disc: Posterior herniation of the disc through a partial defect in the annulus fibrosus. Only the most peripheral or posterior annulus fibers (Sharpey's fibers) are intact. Herniated or prolapsed disc is associated with the non-herniated portion.
Extruded (burst) disc: Posterior herniation of the disc through a defect in the annulus fibrosus.
Sequestrated disc (free fragment): Extrusion of the nucleus pulposus from a defect in the annulus fibrosus, and the absence of communication between this extruded fragment and the unherniated disc. The fragment may be anterior or posterior to the post. long. lig.a, superior or inferior to the disc space, or rarely intradural.
 As degeneration (disc degeneration) progresses, the nucleus of the disc loses its water content and hardens, the intervertebral disc space narrows, spinal movements decrease, and the distribution of forces applied to the annulus fibrosis located on the outer part of the disc is completely disrupted. The shock absorption and load-carrying ability of the disc decreases. Ossification occurs in the disc itself and new bone formation occurs in the vertebrae.
As degeneration (disc degeneration) progresses, the nucleus of the disc loses its water content and hardens, the intervertebral disc space narrows, spinal movements decrease, and the distribution of forces applied to the annulus fibrosis located on the outer part of the disc is completely disrupted. The shock absorption and load-carrying ability of the disc decreases. Ossification occurs in the disc itself and new bone formation occurs in the vertebrae.
The vertebrae are integrated with each other. For this reason, disc herniation is very rare in the elderly (after the age of 60). In those with degenerative disc disease, excessive forceful movements can cause calcification in the annulus fibers.
This is called spondylosis. This often occurs on the back of the spine. Spondylosis is more common with increasing age. Similarly, as the disc space narrows, excessive loads on the facet joints lead to degeneration in these joints.
The resulting narrowing of the disc space and facet joint hypertrophy causes narrowing of the spinal canal and lateral canals (spinal stenosis) and/or mechanical instability (loss of spinal stability), which may lead to nerve root irritation.
Asymmetric loss of lumbar disc height can progress to asymmetric deformation of the spine. If this lateral bending (scoliosis deformity) occurs and progresses, it is together with rotation of the spine. As a result, degenerative scoliosis is seen in advanced ages as a result of severe degenerative changes or due to previous surgeries.
Low Back Pain and Degenerative Disc Disease Symptoms
Low back and leg pain
Remaining in any one position (sitting, standing, or lying down) for too long typically increases pain, requiring frequent position changes. Cough, sneeze or straining Pain is aggravated by flexing the knee and hip (e.g. sleeping with a pillow under the knee) and pain is reduced. Pain may occur spontaneously.
Because the pain threshold is lowered, normally painless stimuli may cause pain (allodynia). The response to the stimulus may be both continuous and exaggerated in amplitude (hyperalgesia). The sensation of pain may be referred to healthy areas.
Motor, sensory and/or reflex changes in the area innervated by the relevant nerve root in the lower extremity.
Neurogenic claudication
Pain in the hip, thigh, or leg on one or both sides with walking, increased tingling and numbness, sometimes loss of strength, relief of symptoms by sitting, squatting or lying down. It is often seen in patients with lumbar stenosis and often begins after the 5th decade.
Lower urinary tract symptoms
Decreased bladder sensation is the earliest finding; later it is not uncommon to see “irritative” signs, including urinary urgency and increased postmicturition residue; less frequently enuresis and dribble incontinence are described in radiculopathy.
Cauda equina syndrome (very rare)
Sphincter disorders, urinary incontinence, inability to urinate, significant sensory deficit in the lower extremities, loss of strength,
Treatment
Conservative treatment: This term is used for nonsurgical treatment. Similar approaches can be used for acute disc herniation, with minor modifications. Most patients only require short-term treatment requires, the treatment is successful.
- Rest cure; 1-2 weeks of bed rest at home, allowing non-strenuous activity in toileting, bathing, and eating; in the absence of radiculopathy, LBP can be well treated with just a few days of bed rest.
- Medication; analgesics are effective but of limited use due to the development of tolerance (mild narcotics for the short term initially), anti-inflammatories (NSAIDs), myelin laxatives (if muscle spasm is present), and sedatives may be used; they should not be used for more than 2-3 weeks.
- PhysiotherapyDifferent methods such as exercise programs, traction, diathermy, hot or cold applications, ultrasound, TENS applications are used.
- Education; proper posture, sleeping positions, lifting techniques. Gradual return to active life. Gradual start of non-intensive exercises.
- Manipulation; is the most controversial treatment method.
- Use of corset: may increase pain
After 1-2 weeks of rest, the maximum benefit will be achieved and then problems (weakness, joint stiffness…) may start from prolonged immobilization. At this point, a physical therapy program may be considered.
Surgical treatment: If conservative treatment fails when disorders such as lumbar disc herniation or lumbar spinal stenosis are detected, surgical treatment directed at the underlying pathology can be performed. It should be noted that surgical interventions subsequently increase degeneration. In the absence of urgent indications for surgery (cauda equina syndrome and progressive or acute severe motor deficit), some time (up to 3 months) can be allowed for resolution of symptoms.